Abstract
Introduction.
Paroxysmal nocturnal hemoglobinuria (PNH) is associated with thrombosis and bone marrow failure. Thrombosis is the leading cause of death and morbidity, with 29-44% of patients presenting at least one thrombotic episode during their disease's natural course. Treatment with complement inhibitors is a strategy associated with reducing up to 80% of thrombosis risk, and improving survival of PNH patients. However, the high cost of these therapies limited their access in Low and Middle-Income Countries (LMIC).
Mexico, like other LMIC, experience low access to complement inhibitors. Hence, we established a primary thromboprophylaxis strategy in classic PNH. The primary objective of the present study is to analyze thrombosis-free survival and all-cause mortality in patients with classic PNH subjected to this prophylaxis strategy compared to historical controls.
Methods.
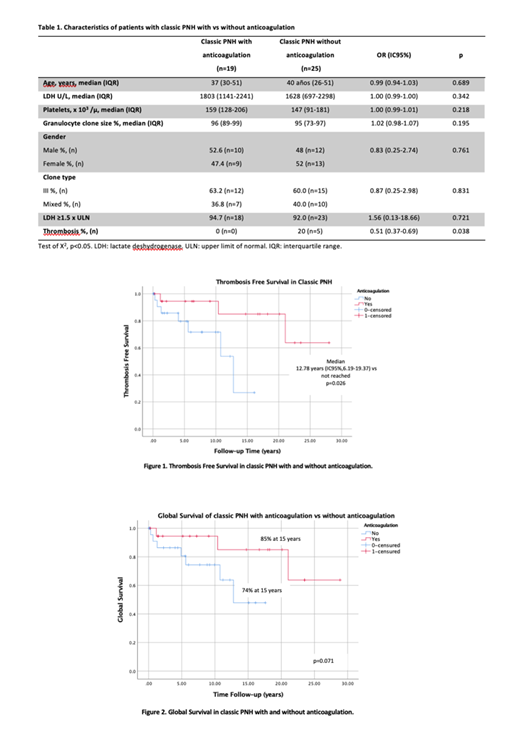
Single-center, retrospective, case-control study. We included patients treated from 1991 to 2021, diagnosed with classic PNH (clone size ≥50% determined by flow cytometry). We defined the treatment group as patients who received total oral anticoagulation as primary prophylaxis. We excluded patients who had presented thrombosis prior to classic PNH diagnosis, sub-clinic PNH, bone marrow failure, platelets <50x10 3/µ, and patients who failed to maintain a therapeutic (2 to 3) INR value three months after starting total oral anticoagulation with vitamin K antagonists (VKA). We collected data regarding clone type (II, III, or mixed), clone size, LDH values (<1.5 vs ≥1.5 x ULN), platelet count, thrombosis occurrence, thrombosis site, bleeding cases and their severity according to the international society on thrombosis and haemostasis (ISTH) classification, and causes of death.
Results.
We found 44 patients with classic PNH diagnosed from 1990 to 2021. Median age at diagnosis was 39 years (28 -51), 50% were female, median LDH value 1669 U/L (926-2,241), and median clone size 95% (80-99). Clone type III was most prevalent, with 61.36% cases, followed by mixed type II-III with 38.64%; we found no type II clone patients. Median follow-up was 21.03 years. Four patients developed a site of thrombosis; three cases (75%) presented simultaneous venous and arterial thrombosis, and one (25%) venous only. The most common site for thrombosis was the portal vein (n=3), followed by supra-hepatic veins (n=1).
A total 19 patients (43.2%) received primary prophylaxis with total oral anticoagulation, 17 (89.5%) used VKA and 2 (10.5%) direct oral anticoagulants. We found no differences regarding age, LDH value, clone size and clone type between the treatment and control groups. There were no cases of thrombosis in the treatment group, while 5 patients (20%) in the control group developed thrombosis at some point (p=0.038, Table 1). Thrombosis-free survival was not reached in the treatment group, vs 12.78 years (IC95%,6.19-19.37) in the control group (p=0.026, Figure 1). Bleeding episodes occurred in 15.8% (n=3) of the treatment group patients, all of them minor according to the ISTH classification.
The global survival was 85% at 15 years in the anticoagulation group vs 74% at 15 years in the control group, (p=0.071, figure 2). Mortality was 15.8% (n=3) in the treatment group vs 28.0% (n=7) in the control group, p=0.338. The only cause of death in the treatment group was progression to aplastic anemia. Causes of death in the control group were thrombosis (28.6%, n=2), aplastic anemia (28.6%, n=2), acute leukemia (14.2%, n=1), sepsis (14.2%, n=1) and digestive tract bleeding (14.2%, n=1).
Discussion and conclusions.
Thrombosis is the most frequent cause of morbidity and mortality in classic PNH patients. In 2003, Hall et al. found that primary prophylaxis with full-dose oral anticoagulation drastically reduced the thrombotic risk in these patients (0 vs. 36.5%, p=0.01). Meanwhile, complement inhibitor has become the mainstay therapy, thromboprophylaxis with oral anticoagulation has virtually stopped in countries where this therapy is accessible. The present study replicated the Hall et al. results, and demonstrated that primary thromboprophylaxis is safe and effective in reducing the risk of thrombosis. In LMIC, where access to complement inhibitors is limited, the use of thromboprophylaxis could abate thrombosis and should be taken in consideration in all patients. Hence, the clonal progression would become the leading cause of death.
Apodaca Chavez: Abbvie: Speakers Bureau; Asofarma: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau. Rangel-Patiño: Abbvie: Speakers Bureau; Bristol: Consultancy. Demichelis: Jazz: Consultancy; Novartis: Consultancy, Research Funding, Speakers Bureau; ASH: Research Funding; Astellas: Consultancy; Gilead: Consultancy; Abbvie: Consultancy, Speakers Bureau; Bristol/Celgene: Consultancy, Speakers Bureau; AMGEN: Consultancy, Speakers Bureau.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal